There are currently NO national/international guidelines that standardise practice and provide framework to support health professionals working with women who wish to return to running after having a baby. This is why the Return to running postnatal guidelines have been published by Grainne Donnelly, Emma Brockwell and Tom Goom. Since their guidelines have been published in March 2019 they have been used by many countries all over the world.
Athletics NI realise what a great opportunity it is for females to be able to access this research and for us to help you put them into practice.
Athletics NI have been working through the Return to Running Guidelines to pull out the most relevant information for those wanting to return to running - while remembering that ONCE A WOMAN IS POSTPARTUM THEY ARE ALWAYS POSTPARTUM and that you can start working on your Pelvic Health at any age. Your body takes time to heal after having a baby, it can take up to 15 months for everything to return to normal.
Looking after your pelvic health is also very relevant for females who are pre and post menopausal.
Athletics NI have put together the following guidelines based on the research by Tom Goom, Gráinne Donnelly and Emma Brockwell, in their 'Returning to Running Postnatal Guidelines for Medical, Health and Fitness Professionals Managing this Population'. You can read their full document here.
The below information is a condensed version of the 'Return to Running Guidelines' from March 2019.
Why do we run?
People run for a variety of reasons- to keep fit; to reach their distance goals; for their mental health; for those tempting endorphins; or simply for the social aspects the running community can bring. Whatever your reason, getting back into running after pregnancy can be a challenge and if you needed more motivation 'Running with a buggy increases your calorie burn by 20%’ https://www.telegraph.co.uk/health-fitness/body/on-your-marks-get-set-5-of-the-best-running-buggies/
What do we do?
At Athletics Northern Ireland, we host our twice-weekly in Belfast and once in Banbridge Buggy Club NI sessions for parents or guardians of young children who are keen to get active. We offer a range of running and core exercises, in a safe and friendly environment.
Below you will find information on assessing your pelvic health; examples to do before returning to running; objective measures for pelvic floor strength; examples of exercise progressions to do before returning to running and Tips for Running with a Buggy.
Assessment of Pelvic Health
Running is a high impact sport placing a lot of demand on your body. To be 'run ready' your body needs time to heal and regain its strength after having a baby.
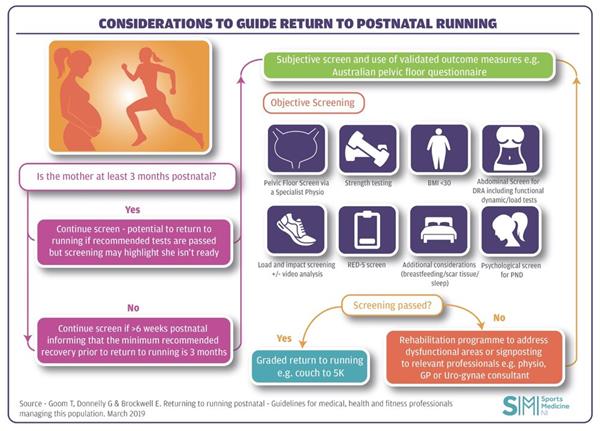
Return to running is not advisable if any of the following subjective or objective issues are identified during screening.
Subjective symptoms: if any of these symptoms are experienced prior to or after attempting return to running then you should contact a pelvic health physiotherapist (page 12 of guidelines)
Objective measures for pelvic floor (page 14 of guidelines)
These tests are preformed by a health professional. The consensus of this guide is that running is less advisable if there is lower than Grade 3 Modified Oxford Manual Muscle Testing (MOMMT- Grade 3: able to contract your pelvic floor through full range against gravity) score during digital vaginal (Laycock and Jerwood 2001) or ano-rectal examination. Testing in both crook lying and functional positions, e.g. standing, is recommended to get a true indication of pelvic floor function and pelvic organ support.
If you have reduced pelvic floor muscle endurance, use the recommended guidelines below as a baseline for starting pelvic floor exercises:
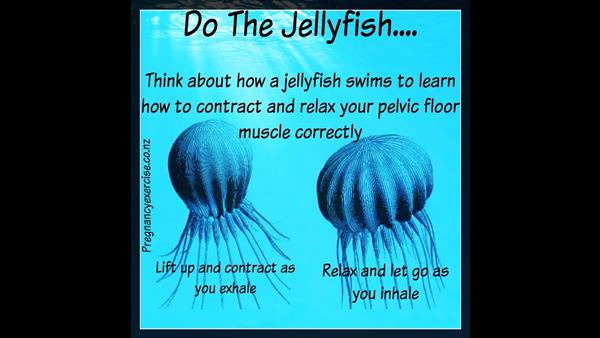
Here are a few cues to help you engage your pelvic floor, courtesy of White Circle
Additional factors for consideration (pages 18 – 23 on the guidelines)
The following factors must be taken into consideration as part of the postnatal evaluation
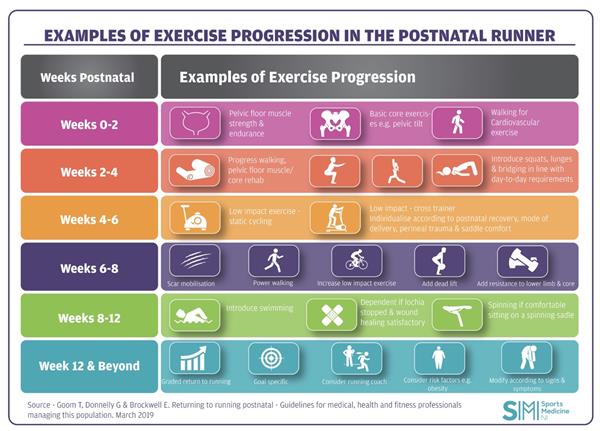
Week 0 to 2
Week 2 to 4
Week 4 to 6
Week 6 to 8
Weeks 8 to 12